ADHD and Hormones: What Every Woman with ADHD Needs to Know
If you're a woman with ADHD, you’ve probably noticed that your symptoms can change based on many factors, including hormonal shifts. Research shows that hormones, especially estrogen, play a significant role in how ADHD symptoms appear (Littman et al., 2021). Understanding how your hormones affect ADHD can help you manage your energy, focus, and mood better, improving your quality of life.ADHD and Hormones: Quick Overview
Women with ADHD often have different symptom patterns compared to men because of hormonal changes. Hormones like estrogen and progesterone control mood and thinking and rise and fall at various stages of life. These changes can make ADHD symptoms better or worse. Knowing these patterns can help you manage symptoms more effectively (Rucklidge, 2010).Estrogen and Dopamine: How They Affect ADHD
Estrogen is connected to dopamine, a brain chemical that helps control focus, mood, and attention—things that are usually hard for people with ADHD. When estrogen levels are high, dopamine works better, which makes it easier to concentrate and feel emotionally balanced (Littman et al., 2021). When estrogen levels drop, such as before your period or during menopause, you might feel more distracted, forgetful, and moody.Progesterone and Other Hormones: Their Role in ADHD
Besides estrogen, other hormones like progesterone and testosterone also affect ADHD symptoms. Progesterone can calm the brain but can also cause tiredness or "brain fog" when levels are high (Liisa, 2019). Understanding that these hormones work together can give you a clearer picture of how your symptoms change. Researchers are building on their understanding of precisely how hormone interactions at different stages of the cycle might impact women.According to the hormone sensitivity theory, women with ADHD may be more vulnerable to impulsivity and risk-taking during mid-cycle (high estrogen) and experience inattention, mood swings, or negative emotions toward the end of the cycle (low estrogen and high progesterone) (Eng et al., 2024).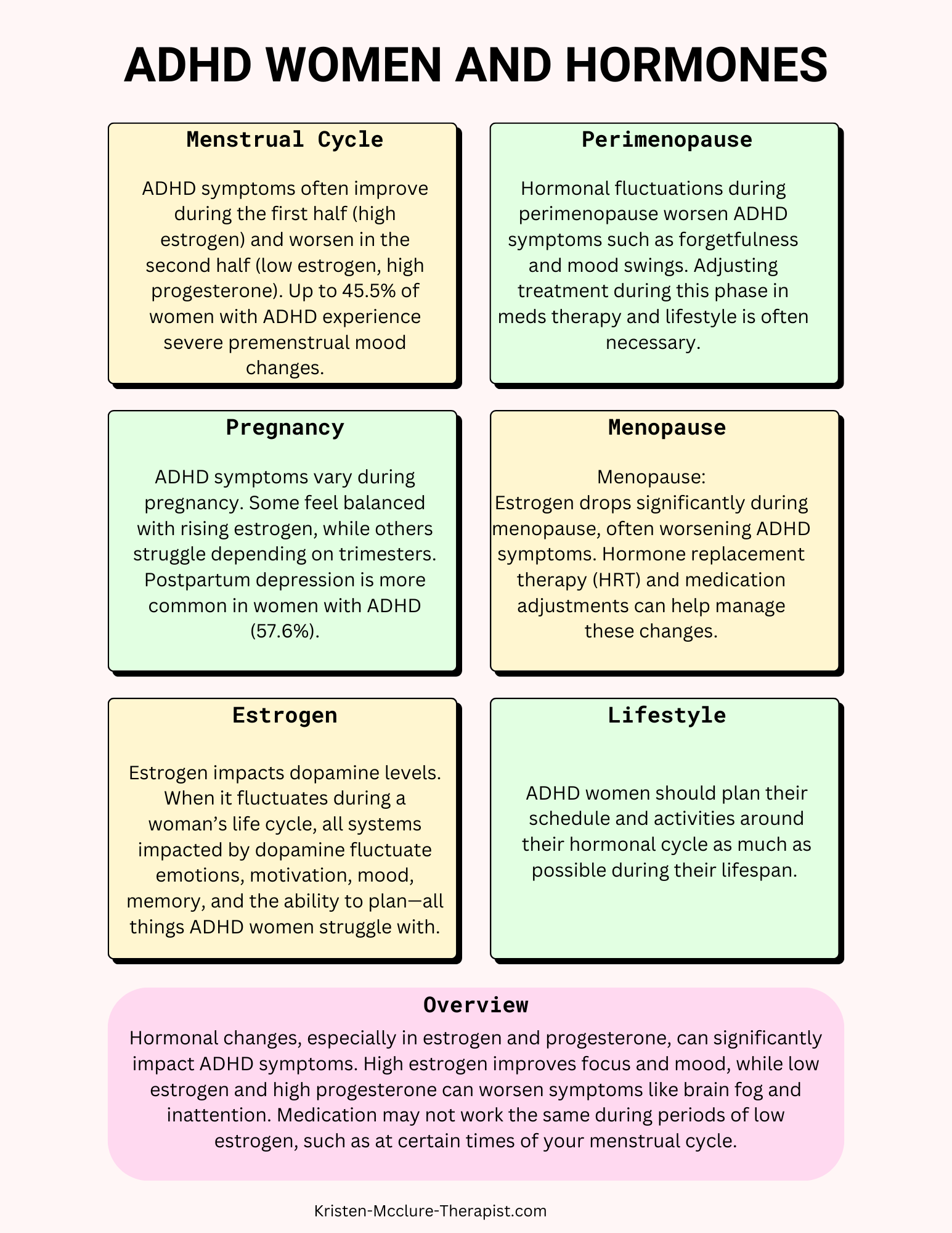
ADHD, Hormones, and Your Menstrual Cycle
Your menstrual cycle has two main phases: the follicular phase, when estrogen levels rise, and the luteal phase, when estrogen drops. Many women with ADHD notice their symptoms get worse in the luteal phase, right before their period. Studies show that up to 45.5% of women with ADHD experience severe premenstrual mood changes, which is higher than in women without ADHD (Dorani et al., 2021). Keeping track of your cycle can help you predict and manage these symptom changes. [Learn more about ADHD and your menstrual cycle here.]ADHD, Hormones, and Pregnancy
During pregnancy, estrogen levels rise a lot, which might help some women with ADHD feel more balanced and calm. However, many women with ADHD struggle with mood swings and increased responsibilities, which can make ADHD symptoms harder to manage. About 57.6% of women with ADHD experience postpartum depression, a rate much higher than in women without ADHD (Dorani et al., 2021). It’s important to talk to your doctor about managing ADHD during pregnancy. [Read more about ADHD and pregnancy here.]ADHD, Hormones, and Perimenopause
Perimenopause is the transition phase before menopause, when hormone levels rise and fall a lot. Many women with ADHD find that this makes their symptoms, like forgetfulness and mood swings, worse (Littman et al., 2021). Even if you’ve managed your ADHD well before, perimenopause can make it harder to control. Working with your doctor to adjust your treatment plan can help during this time. [Find out more about ADHD and perimenopause here.]ADHD, Hormones, and Menopause
Menopause happens when your body stops having periods, and estrogen levels drop a lot. This can make ADHD symptoms like anxiety, trouble focusing, and mood swings worse (Craig et al., 2020). There are ways to manage these changes, like hormone replacement therapy, lifestyle changes, and adjusting ADHD treatments (Littman et al., 2021). Working with your doctor can help you find the best approach. [Discover more about ADHD and menopause here.]ADHD Medications and Hormonal Fluctuations
As your hormone levels rise and fall, your ADHD medication might work differently. Many women find they need to adjust their medication based on where they are in their hormonal cycle. This is especially true during perimenopause and menopause, when some women feel their ADHD medications aren’t as effective (Craig et al., 2020). It’s important to talk to your doctor about making adjustments to your medication during these times.Coping Strategies for Hormonal Shifts
In addition to tracking your cycle and working with your doctor on medication adjustments, there are lifestyle strategies that can help manage ADHD symptoms during hormonal changes.
Regular exercise, enough sleep, reducing stress, and eating a balanced diet can all help support your focus and mood. Mindfulness, neurodivergent affirming cognitive behavioral therapy (CBT), and hormone replacement therapy (HRT) are other options that may provide relief (Haimov-Kochman et al., 2019).
Using symptom-tracking tools or apps that let you monitor your feelings during different phases of your cycle can also help. This information will allow you to adjust your self-care and treatments to what works best for you.
Empowering Yourself with Knowledge and Support
Understanding how hormones affect your ADHD symptoms is critical to managing them better at different stages of life. You’re not alone in navigating these changes—there are many resources and communities out there that can help you. You can live a more balanced and fulfilling life by staying informed, tracking your symptoms, and speaking up for the care you deserve.References for ADHD Women and the Impact of Hormones
- Babinski, D. E., Pelham, W. E., Molina, B. S., Waschbusch, D. A., Gnagy, E. M., Yu, J., Sibley, M. H., & Biswas, A. (2011). Women with childhood ADHD: Comparisons by diagnostic group and gender. Journal of Psychopathology and Behavioral Assessment, 33(4), 420–429.
- Bro, A. (2020). Managing ADHD During Pregnancy. Journal of Women's Health, 29(4), 531-539. https://doi.org/10.1089/jwh.2019.7803
- Craig, M., Davies, N., & Cooper, P. (2020). ADHD and the Role of Estrogen in Cognitive Function. Psychoneuroendocrinology, 118, 104709. https://doi.org/10.1016/j.psyneuen.2019.104709
- Dorani, F., Bijlenga, D., Beekman, A. T. F., van Someren, E. J. W., & Kooij, J. J. S. (2021). Prevalence of hormone-related mood disorder symptoms in women with ADHD. Journal of Psychiatric Research, 133, 10-15. https://doi.org/10.1016/j.jpsychires.2020.12.005
- Eng, A. G., Nirjar, U., Elkins, A. R., Sizemore, Y. J., Monticello, K. N., Petersen, M. K., Miller, S. A., Barone, J., Eisenlohr-Moul, T. A., & Martel, M. M. (2024). Attention-deficit/hyperactivity disorder and the menstrual cycle: Theory and evidence. Hormones and Behavior, 158, 105466. https://doi.org/10.1016/j.yhbeh.2023.105466
- Littman, E., Dean, J. M., Wagenberg, B., & Wasserstein, J. (2021). ADHD in Females Across the Lifespan and the Role of Estrogen. The ADHD Report, 29(5), 1-6.
- Rucklidge, J. J. (2010). Gender Differences in ADHD: Implications for Diagnosis and Treatment. Neuropsychiatric Disease and Treatment, 6, 563-571. https://doi.org/10.2147/NDT.S6620