Is ADHD a Trauma Response? Clearing Up the Confusion
If you’re a woman with ADHD, you’ve likely encountered the question: Is ADHD caused by trauma? This belief can sound convincing at first—after all, ADHD and childhood trauma share overlapping symptoms, like trouble focusing or regulating emotions. However, this oversimplified explanation doesn’t hold up under scrutiny. ADHD is not caused by trauma.
While trauma can worsen ADHD symptoms or mimic them, ADHD is a neurodevelopmental disorder rooted in genetics and brain biology. Misunderstandings around this topic—often perpetuated by well-known figures like Gabor Maté—have contributed to the confusion. Let’s break it down.
Where Did the Myth Come From?
The myth that ADHD is a trauma response partly stems from research showing how early trauma impacts brain development. Dr. Bessel van der Kolk’s widely-read book, The Body Keeps the Score, highlights how ADHD and childhood trauma can disrupt the ability to regulate emotions, focus, or stay calm—experiences that overlap with ADHD symptoms.
Adding to this, Gabor Maté has emphasized how adverse childhood experiences shape adult struggles, including ADHD-like traits. Maté suggests that childhood stress and attachment issues play a significant role in the development of ADHD. While this perspective resonates with many, it overshadows decades of evidence showing ADHD’s neurodevelopmental origins.
The truth is, trauma can shape how ADHD presents, but it does not create ADHD. ADHD is primarily a genetic condition linked to differences in brain structure and function, particularly in regions responsible for focus, impulse control, and emotional regulation.
What Does the Science Say?
ADHD’s Biological Roots:
- Genetics: ADHD runs in families. If a parent has ADHD, there’s a high likelihood their child will, too.
- Brain Structure: Neuroimaging studies reveal differences in the size and activity of certain brain areas in people with ADHD, especially the prefrontal cortex, which governs planning and attention.
- Neurotransmitters: ADHD brains process dopamine and norepinephrine differently, which impacts motivation, reward systems, and impulse control.
Trauma’s Impact:
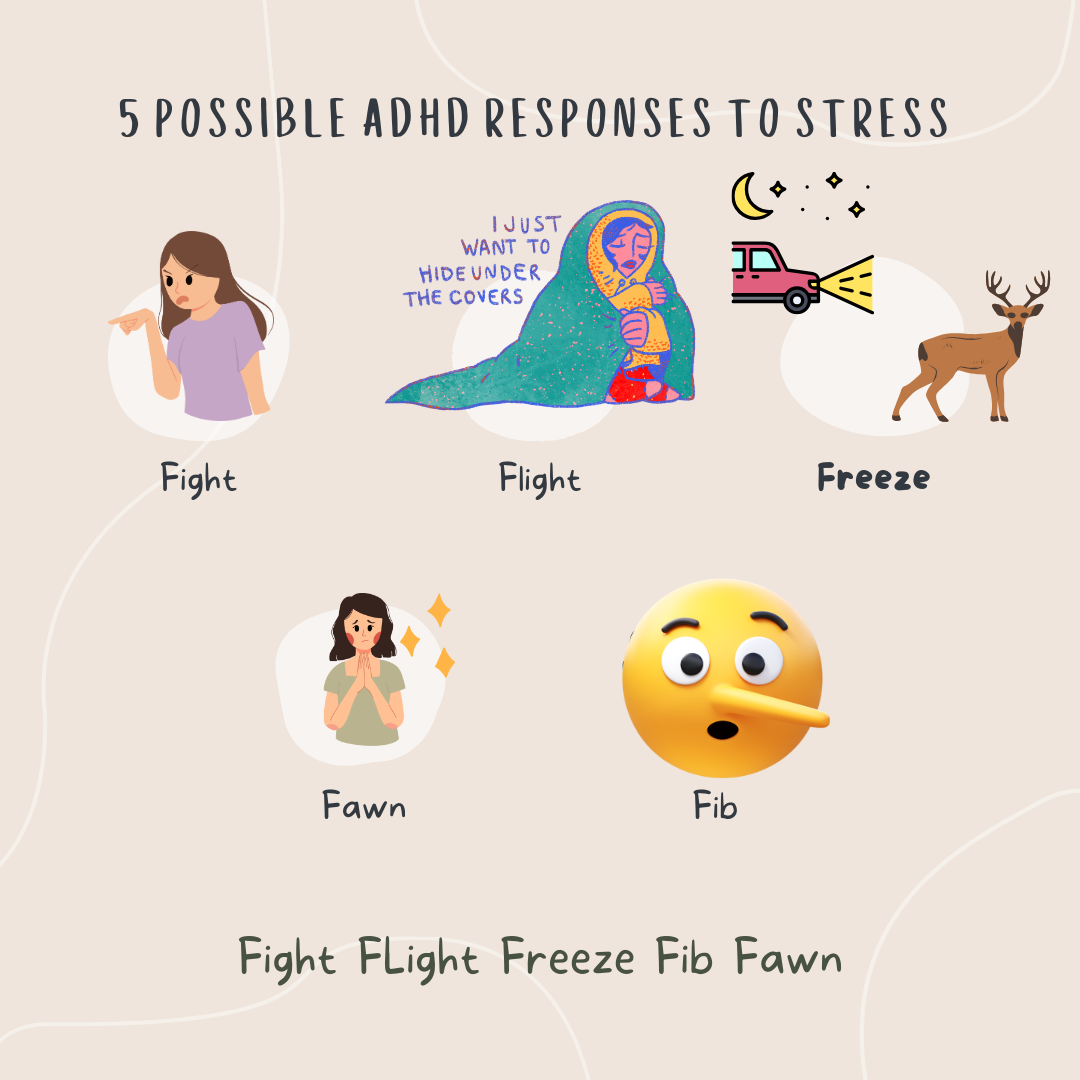
- Trauma doesn’t alter brain structure in the same way as ADHD. Instead, it disrupts stress response systems, keeping the brain in a state of heightened alert (fight, flight, or freeze).
- Trauma-related symptoms are often tied to specific events and can fluctuate with triggers, unlike the consistent, lifelong traits of ADHD.
While trauma can exacerbate ADHD struggles—like emotional dysregulation or focus issues—it doesn’t change the underlying wiring of an ADHD brain.
Why Does This Misconception Persist? Gabor Mate and The Idea that ADHD is a Trauma Response.
Figures like Gabor Maté have played a role in perpetuating this myth. His work highlights the effects of childhood adversity on mental health, suggesting that the way parents respond to children’s needs during formative years contributes to the development of ADHD.
While this lens can help people understand how environmental factors influence behavior, it oversimplifies the complexity of ADHD. By focusing so heavily on external causes, it overlooks the genetic and neurological evidence that firmly establishes ADHD as a neurodevelopmental condition.
This confusion can be harmful. For one, it may discourage people with ADHD from seeking treatments like medication or coaching, believing instead that resolving past trauma will “fix” their ADHD. While addressing trauma is important, it’s not the same as managing ADHD.
How Are ADHD and Trauma Different?
| Feature | ADHD | Trauma Response |
|---|---|---|
| Cause | Neurodevelopmental: genetic and brain-based. | Environmental: caused by distressing experiences. |
| When Symptoms Start | Present from birth noticeable in childhood | Begin after a traumatic event. |
| Consistency | Present in all environments, though intensity may vary. | Symptoms tied to triggers or reminders of the trauma. |
| Treatment | Neurodivergent therapy, ADHD coaching, CBT, or medication. | Trauma-focused therapy (e.g., EMDR, IFS, or somatic therapy). |
What This Means for ADHD Women
If you’ve ever wondered whether your ADHD was caused by trauma, know this: ADHD is not a trauma response. It’s part of how your brain works—a neurotype with unique strengths and challenges. Trauma can intensify ADHD struggles, but it doesn’t define or create them.
This distinction is crucial for women with ADHD because:
- It Reduces Shame: ADHD is not a result of what happened to you or how you were raised. It’s part of who you are.
- It Ensures Proper Treatment: ADHD-specific treatments—like coaching, medication, or neurodivergent therapy—address the brain’s unique wiring in ways trauma therapy alone cannot.
- It Empowers You: By embracing ADHD as a neurotype, you can focus on building environments that support your brain and allow your strengths to shine.
Healing from Trauma While Thriving with ADHD
For women who experience both ADHD and trauma, it’s important to address each issue in a way that respects their differences:
- For ADHD: Strategies like medication, neurodivergent therapy, and ADHD coaching can help with focus, impulsivity, and executive functioning.
- For Trauma: Treatments like EMDR, Internal Family Systems (IFS), or somatic therapy can help process past experiences and regulate the stress response.
Both journeys are valid, and healing in one area can often improve the other. For example, processing trauma can make it easier to manage ADHD-related emotional dysregulation, while ADHD tools can reduce overwhelm during trauma work.
The Bottom Line
ADHD is not a trauma response. It’s a neurodevelopmental condition rooted in genetics and brain biology. Trauma may influence how ADHD shows up or is managed, but it doesn’t cause ADHD.
Understanding this distinction allows women with ADHD to advocate for themselves, seek appropriate treatments, and embrace their neurodivergent strengths. Healing from trauma and thriving with ADHD are both possible—and neither journey invalidates the other.
What’s your experience with ADHD and trauma? Have you encountered this myth in your own life? Share your thoughts in the comments, and let’s continue breaking down misconceptions together.